In my previous post, we examined five critical features you should consider when selecting clinical episode grouping technology for your organization.
Today, we’ll discuss four use cases where a modern, AI-powered grouper can drive significant financial savings while improving your population’s health, well-being, and productivity.
The Problem with Standard, Legacy Groupers
Many of the standard, commercially available clinical episode groupers were built in the 1990s, and are not well equipped to organize data for modern, advanced machine learning.
These tools were designed to support provider profiling, rudimentary population health management, claim payment, and basic condition-focused reporting. They can answer questions such as, “How many patients with chronic diseases are in my population?”
But what if you want to take your analytic insights to the next level? What if you want to really understand what’s happening within the confines of your population’s morbidity? What if you want to identify areas of opportunity and avoidable overspending, and take proactive steps to boost health and well-being?
The Solution: A Modern Grouper Built for the Age of AI
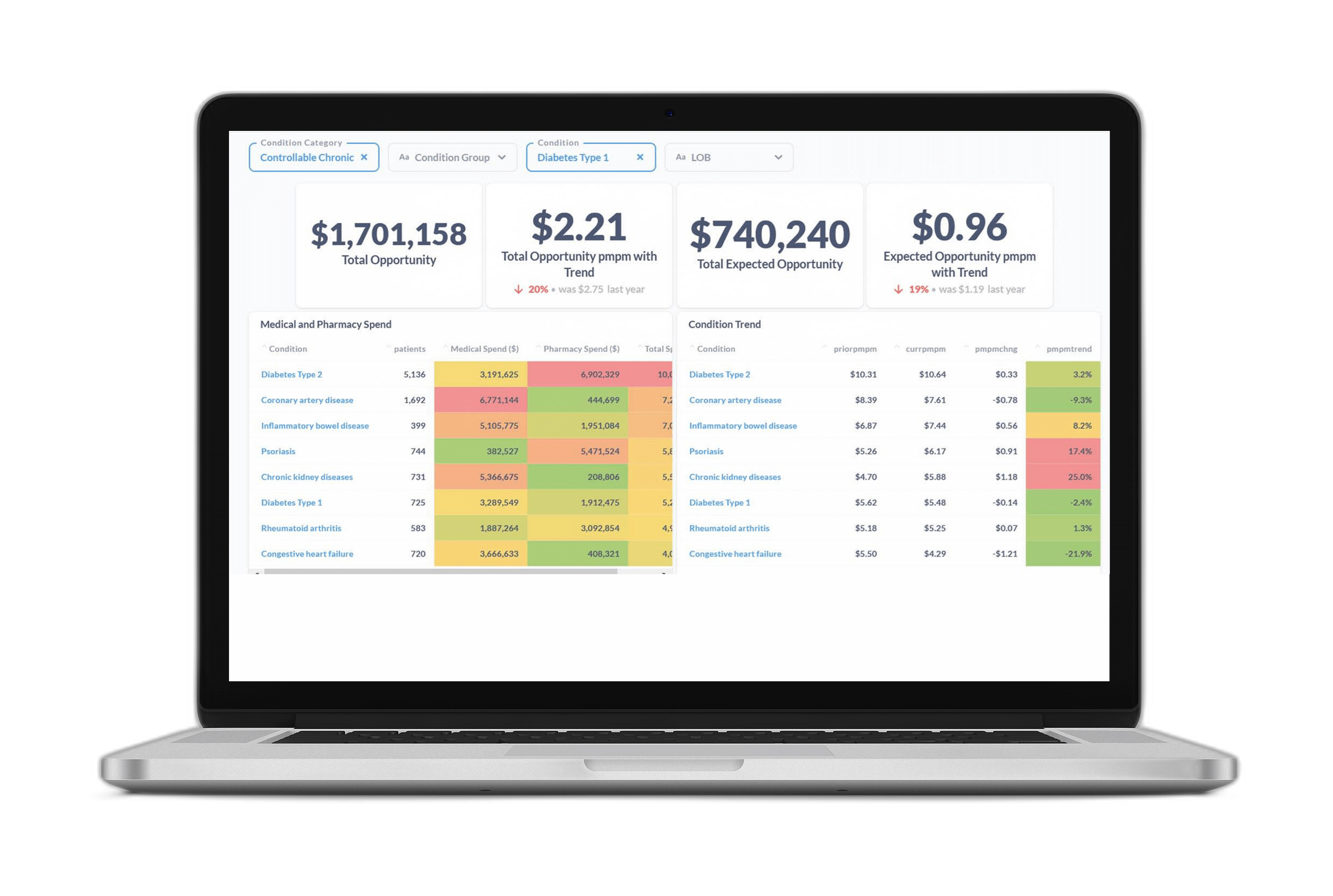
A robust, modern episode grouper such as Certilytics’ CORE Pathways— that was built to organize data for advanced predictive analytics—can provide deep insights to drive better business decisions. This is true whether you’re a payer implementing clinical management programs, an employer trying to understand whether you’re getting value from your vendor partners, or a provider bearing risk for managing certain aspects of a population.

Here are four examples of how our customers have taken their organizations to the next level through the adoption of CORE Pathways:
Use Case 1: Large Claimant Predictions
Nothing wreaks havoc on a healthcare budget more than an unexpected influx of large claims. Even with specific and aggregate reinsurance, the ceded portion of the liability can quickly add up if a plan experiences more large claims than anticipated.
An episode grouper like CORE Pathways that combines the clinical and financial attributes of each these large claims can significantly increase the accuracy of high cost claimant predictions. Indeed, each patient’s medication history and treatment regimen, high cost event triggers such as hospital admissions and surgeries, and high-risk comorbidities all contribute to understanding if a large claim is imminent. It is imperative that your episode grouper be able to identify all of these conditions and services, so that actuaries and underwriters are armed with the most accurate predictive insights possible, and can reduce uncertainty in a plan’s future liabilities.
Use Case 2: Identify Member Level Treatment Pathways
Every patient’s treatment pathway is unique, and will vary based on their PCP, which specialists they are referred too, their location, comorbidities, medications, severity, etc. A critical part of accurately predicting outcomes for different population cohorts is having the ability to understand where each patient has been in their journey and where they are likely headed based on their unique characteristics.
CORE Pathways accomplishes this by focusing not just on retrospective utilization, but also making predictions through integrated, patient-level, condition, and service-centric AI-powered models. With these prospective insights, users can quickly analyze both past and future costs, improve upon the way they risk stratify their population, and identify earlier interventions to help manage member and provider behavior.
Use Case 3: Provider Practice and Billing Patterns
Much attention is placed on measuring care quality by specialists—and rightfully so. While cost is considered in conjunction with quality metrics, the primary drivers of the cost variations between specialists are often not measured or understood, and are frequently explained away as a component of risk adjustment.
However, more often than not the real culprit is the variation in practice patterns and billing patterns. To put it another way, one specialist might be billing for more services than other specialists in the region to treat the same condition. A key advantage of CORE Pathways is that it organizes the data to allow for these variations from the norm to be measured, explained, and quantified.
Use Case 4: Analytics as a Value-Added Service
As price transparency legislation continues to evolve, the tried and true mechanisms for managing unit cost will become less important, with market forces driving reimbursement rates to be more consistent across payers. This underscores the need for sophisticated analytic tools and grouping methodologies, as risk-bearing entities look for other means to manage the healthcare dollar and highlight their value proposition beyond lowest achieved discounts and the broadest network.
Conclusion
If your grouper can’t deliver these kinds of analytics, it may be time to consider alternatives.
Organizations armed with the information outlined above will be able to provide their customers and constituents with a much deeper understanding of the populations they manage.
To learn more about Certilytics reach out to us for a free consultation with our team of experts at contact@certilytics.com.